Authors: Usama Bin Saeed ( Department of Orthopedic Surgery, Allied Hospital, Punjab Medical College, Faisalabad. )
Rana Dawood Ahmad Khan ( Department of Orthopedic Surgery, Allied Hospital, Punjab Medical College, Faisalabad. )
Muhammad Zain-ur-Rehman ( Department of Orthopedic Surgery, Allied Hospital, Punjab Medical College, Faisalabad. )
Ajmal Yasin ( Department of Orthopedic Surgery, Allied Hospital, Punjab Medical College, Faisalabad. )
November 2015, Volume 65, Issue 11
Original Article
Abstract
Background: Total hip arthroplasty is a common and successful treatment for osteoarthritis of the hip. Demographic trends in Pakistan suggest a significant increase in the demand for total hip replacement surgery.
Objectives: The current study was planned to assess the outcome of THA at our centre in terms of pain relief and functional improvement by using pre and postoperative HHS. It was observed in this study that the functional outcomes were highly encouraging. Patients were handicapped because of pain, loss of movements and inability to carry out day-to-day activities due to arthritis of the hip joint. The same functional improvements were noted from examination of the patients according to Harris Hip Score.
Patients and Methods: The descriptive case series was conducted at Punjab Medical College and affiliated hospitals from July 2013 to July 2014, and comprised patients of either gender 25 years or more of age with primary or secondary OA of hip. Severe complications in total hip replacement comprise dislocation, aseptic loosening, infection, peri-prosthetic fracture and limping. Time period of this study was short so a longer period of follow-up is suggested for better evaluation.
Results: Mean pre-operative HHS was 31.88+7.43 and post-operatively it was 81.23+9.56 which meant good results with marked improvement.
Conclusion: The study concluded that total hip arthroplasty is a secure procedure with tremendous benefits
Keywords: Total hip arthroplasty, Harris hip score, Osteoarthritis, Ankylosing spondylitis, Functional class. (JPMA 65: S-190 (Suppl. 3); 2015)
Introduction
Total hip arthroplasty (THA) is a common and successful treatment for osteoarthritis of the hip. Demographic trends in Pakistan suggest that in the decades ahead a significant increase would be seen in the demand for total hip replacement surgery. The 20-year survival of a total hip prosthesis is approximately 85%.1 The hip joint is a ball and socket synovial type joint between head of the femur and acetabulum of the pelvis. It joins the lower limb to the pelvic girdle. The hip joint is designed to be a stable weight-bearing joint. To achieve this, a large range of motion (ROM) is sacrificed for stability.
Arthroplasty is a surgical procedure to restore the integrity and function of a joint. A joint can be restored by resurfacing the bones by prosthesis. Various types of arthritis may affect the joints. OA, or degenerative joint disease, is a loss of the cartilage or cushion in a joint, that causes intolerable pain which is the primary indication followed by limited functional ability.
Osteoarthritis (OA) is by far the most common disease of hip with markedly increased prevalence with increasing age.2 It is a group of mechanical abnormalities involving degradation of joints, including articular cartilage and subchondral bone. Symptoms may include joint pain, tenderness, stiffness, locking and sometimes an effusion.
The main cause is limb mal-alignment, combined with hereditary, developmental and metabolic factors, which lead to loss of cartilage, sometimes exposing and damaging the underlying bone. Pain makes it difficult to exercise, so muscles may atrophy. OA is believed to be caused by mechanical stress on the joint and low-grade inflammatory processes. Unlike rheumatoid arthritis (RA), it is not primarily an inflammatory condition.
Treatment begins with weight-loss, exercise and analgesics. If pain becomes debilitating, joint replacement surgery can usually help, though outcomes are sometimes poor.
The major milestones in the treatment of hip arthritis have been acetylsalicyclic acid (ASA) in the mid-1800s with subsequent derivation of non-steroidal anti-inflammatory drugs (NSAIDs).3
Various systems of pre and post-operative assessment of hip are used but the most commonly used system is Harris Hip Scoring (HHS) system.3,4 THA is frequently performed in our setup but still at early stages of growth due to deficiency of properly trained staff, lack of proper operation room facilities, inadequate patient education and high risk of infection. The current study was planned to assess the outcome of THA at our centre in terms of pain relief and functional improvement by using pre and postoperative HHS.
Patients and Methods
The descriptive case series was conducted at Punjab Medical College and affiliated hospitals from July 2013 to July 2014, and comprised patients of either gender 25 years or more of age with primary or secondary OA of hip. Those with previously failed THA, septic arthritis, neuropathic joints, neurological defects around the hip (paralyzed abductors) and congenital defects were excluded.
Non-probability purposive sampling technique was used to enrol patients from the Orthopaedic out-patient department (OPD).
After informed consent from the patients, detailed history, including pain at hip, decreased movement at hip, shortening of limb and limp, was taken. Physical examination included flexion contracture, limb length discrepancy (LLD), ROM, deformity and gait analysis. Pre-operative HHS was noted. Diagnosis was confirmed by antero-posterior and lateral hip X-ray views. Baseline investigations included complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), blood urea nitrogen (BUN), serum urea and creatinine, prothrombin time (PT), activated partial thromboplastin time (APTT), blood sugar, Anti-hepatitis C virus (HCV), and hepatitis B surface antigen (HBsAg).
All patients were operated upon as elective cases. Pre-operative antibiotic (third-generation cephalosporin)was given at the time of induction.
Post-operatively, patients were not allowed to squat and use precautions while using toilet. For pain relief, injectable narcotic analgesics and NSAIDs were given. Injectable antibiotic was continued 8 hourly for 3 days and low molecular weight heparin (Clexane) 40mg subcutaneously was injected once a day for prophylaxis against deep vein thrombosis (DVT) for a week. Physiotherapy was started on the first post-operative day, while drain was taken out when drainage was less than 50ml in 24 hours for 48 hours. Dressing was changed after 48 hours, and Ambulation with the help of walker was started when pain-free. Clexane was stopped after a week, and Patients were discharged on 5th to 7thpost-operative day.
u Patients were evaluated on HHS post-operatively along with X-rays at 04, 08 and 12 weeks.
Pre-op HHS was compared with post-operative scores to see improvement. Increase in HHS of >20 points along with radiographically stable implant with no additional femoral reconstruction was considered a successful result. In terms of grading out of a total 100 score, <70 indicated Poor; 70-79 Fair; 80-89 Good; and 90-100 Excellent.
Pain relief was assessed from0 to 44, according to HHS. Functional class was determined by assessing the limp while walking, use of support while walking, distance walked, ability to climb stairs, putting on shoes and socks, sitting in chair and using public transport. Angles were measured and rated 0 to 4.
Data was analysed using SPSS 19.
Results
Of the 51 patients enrolled, 6(11.7%) were lost to follow-up, and 45(88.2%) completed the study. Of them, 28(62.22%) were males and 17(37.77%) were females. The mean age of the patients was 49.25±10.65 years (range: 25-90 years). Avascular necrosis (AVN) was the most common cause in 21(46.66%) patients (Figure-1).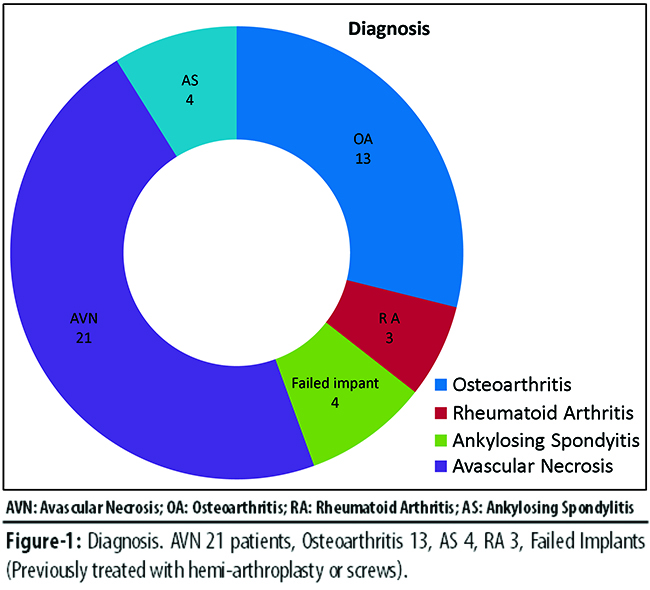
The mean pre-operative ROM score was 2.50±1.01 (range: 0-5). At the last follow-up, it was 4.45±0.74 (range: 4-5). The mean pre-operative deformity score was 2.36±1.67 (range: 0-4).At the last follow-up, it was 4.23±0.01 (Table-1).
Mean pre-operative HHS was 31.88+7.43 and post-operatively it was 81.23±9.56 which meant good results with marked improvement.
Mean pre-operative HHS (Table-2) and mean post-operative HHS in different diseases (Table-3)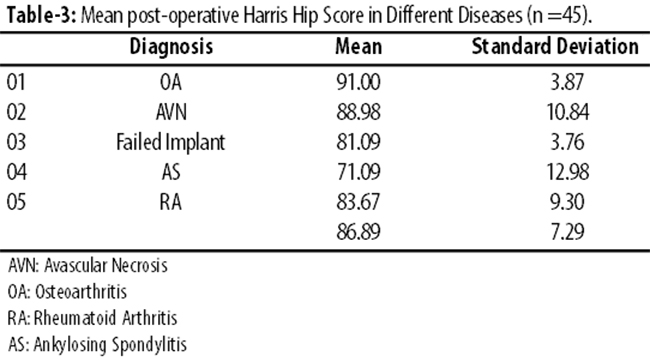
were also compared. Mean improvement in HHS in Osteoarthritis was 71.45±10.43. In AVN it was 63.87±8.54, in Ankylosing Spondylitis (AS) 41.87±8.09, and in RA 70.02±8.94. Infection was the most common complication in 5(11.11%) cases (Figure-2).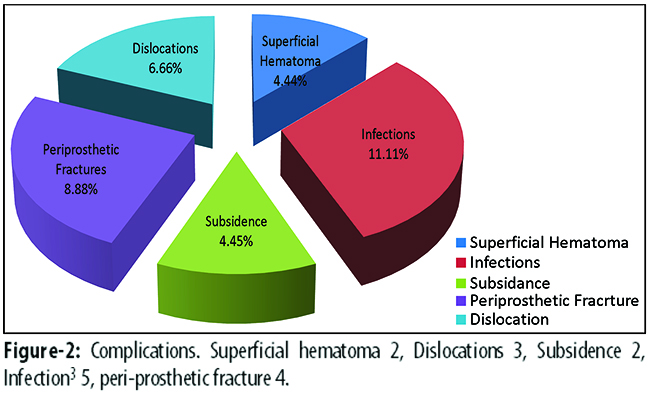
Overall results were Excellent in 27(60%) of the hips, Good for 10(22.22%), Fair for 3(6.66%) and Poor for 5 (11.11%).
Discussion
Total hip replacement (THR) is most commonly used to treat joint failure caused by OA. Other indications include RA, AVN, traumatic arthritis, certain hip fractures, benign and malignant bone tumours, arthritis associated with Paget\\\'s disease, AS and juvenile RA. The aims of the procedure are pain relief and improvement in hip function. Hip replacement is usually considered only after other therapies, such as physical therapy and pain medications, have failed. THA is continuously evolving interms of material, prosthetic design, surgical technique, prevention of complications, and postoperative management. The future of prosthetic hip design lies in the development of new materials that will have acceptable biocompatibility and better physical properties, leading both to better integration into bone and better wear characteristics.5
In our study the average age of the patients at the time of operation was 49.25±10.65 (range 25-90 years). In a study by Michael J et al. the average age of the patients at the time of operation was 52 years.7 In a study by Shahabud-din et al. the average age of the patients was 34 years (range: 19- 49 years).8 In a study by Berli BJ et al, the mean age of the patient at surgery was 67.3 years (range: 49-86 years).9 Study by Ragab et al. reported average age of the patients to be 62.2 years (range: 39-84 years).10 In a study by Todkar M. et al., the average age of the patients was 65 years (range: 50-80 years).11 In a study by Iqbal P et al., mean age was 48 years (range: 21-75 years).12 In a study by Ghani et al, the average age of the patients was 57 years (range: 25-87 years).13 OA of knee and hip present at an early age in South Asia which is most likely due to our sitting, praying, eating and working habits, which require squatting. The use of indoor and outdoor toilets also put excessive stress and strain on knee and hip joints. So patients in our study underwent arthroplasty at a mean age (49.25±10.65) almost a decade earlier than Western societies.
Todkar M et al. reported diagnosis of osteonecrosis of femur head in 39(78%) cases, RA in hip in 1(2%) and OA in 1(2%). Ghani et al. in a study of 20 patients had RA in 35%, OA in 10 %, failed hemi-arthroplasty 25%, and fracture neck of femur 10%. Shabaud-din et al. in a study of 20 total hip replacements, AVN 70%,AS 10%, fracture acetabulum 10% and unknown 10%. In a study by Iqbal P et al., the preoperative diagnosis was secondary OA in 45(62.5%), primary OA 10 (13.89%), AVN 4(5.56%), AS 6(8.33%) and RA7 (9.72%). However, compared to these results, we had AVN 21(46.66%), AS 4(8.88%), OA 13(28.88%), RA 3(6.66%), and failed previous implant 4(8.88%).
The average preoperative HHS in our study was 31.88±7.09 points. In a study by Ragab et al, the average preoperative score was 48 points and it went to 88 post-operatively. Pospischill M et al. reported the latest mean pre-operative score of 41 and post-operative HHS 89.2 (range: 32-100).15 At a mean follow-up of 14.4 years, the clinical ratings were graded as Excellent and Good in 83(80.1%), Fair in 8(7.7%), Poor in 12(11.6%)of all reviewed hips. The mean pain score was 41.6(range: 10-44), with the maximum 44 found in 89(86.4 %) of all the evaluated hips. In a study by Berli BJ et al., the mean pre-operative HHS was 73 and post-operatively it was 96. In a study by Michael J et al., it moved from 51 points to 94 and 86% of the hips had a Good or Excellent result. In a study by Bourne RB et al., the mean post-operative HHS for 131 hips was 89±10 points.16 In a study by Todkar et al., mean preoperative HHS was 43 in patients with AVN, and postoperatively it went on to 88. In rheumatoid hips, the HHS went to 82 from 45. In AS patients, it went from 49 to 83. In OA patients, Mean HHS was 47 and went on to 87 postoperatively.17,18 Improvement in HHS in our study is comparable with these studies and the recorded post-operative score was 81.23±9.56. Pierce TP showed a pre-operative score of 40 and post-operative score of 89 and 92% patients were satisfied with their surgery.19 Post-operative dislocation, a typical early complication, occurs mostly within 3 months after surgery. In uncomplicated cases, incidence of dislocation is 1-2%. However, in cases of revision surgery risk can increase up to 10%.The rate of dislocation reported in much larger series was 3%. In our study there were 3 dislocations and they were managed by closed reduction. In a study by Berli BJ et al., there was one dislocation and it was treated by closed reduction. Shabud-din et al. in a study of 20 total hip replacements reported dislocation rate of 5% that required a reoperation. Iqbal P et al. in a study of 72 hip replacements, reported 7% rate of dislocations.
The incidence of infection after primary THR is 1%. It is expensive and time consuming to treat, and usually results in poor functional outcome. Patients who may be at increased risk include severe RA, on steroids, with previous hip surgery, and persons with history of infection in and about the hip. In the current study, 5 patients had superficial infections that settled within 2 weeks of intravenous (IV) antibiotics. Shahabud-din et al. reported 5% rate of infection. Iqbal P et al. reported 4% And Todkar M et al.,2%.
Subsidence of the femoral component in total hip was defined by the distance measured between the lesser trochanter and the proximal tip of the stem on the pelvic radiograph.20
Subsidence was evaluated by comparing the immediate post-operative radiographic images with those obtained at follow-up. All radiographs were digitalised. Subsidence was measured as a vertical drop of the stem, characterised by a radiolucent line at the proximal most aspect of the cement-prosthesis interface. In a study by Jonathen DJ et al., subsidence occurred in 2 femoral components and was attributed to undersized stems.In a study by Loudon JR and Charnley, subsidence occurred in 26% cases.21 In our study, 2 patients had subsidence and for which a revision surgery of the femoral stem was carried out.
The risk of preoperative femoral fracture has been shown when a cement-less component is used in revision THA. In our study, the rate of peri-prosthetic fracture was 8.88% and they were managed with revision surgery.
In our study 5 patients were infected post-operatively and they were managed with incision and drainage and antibiotics according to culture and sensitivity. Two of them had to undergo revision surgery afterwards due to loosening of their implants.
Venous thromboembolic disease is common following hip arthroplasty. In a study by Alexander et al., the incidence of symptomatic venous thromboembolism was 2.7% (150 of 5607) of which 1.1% had developed pulmonary embolism, 1.5% had deep vein thrombosis (DVT) and 0.5% had both.22 In a study by Erikson et al., incidence of DVT was 0.6% (15 out 2500).23 In our study, there was no incidence of thromboembolism.
Conclusion
Total hip arthroplasty is a secure procedure with tremendous benefits. It improves quality of life in terms of pain relief, movements and functional ability. Immediate complications in total hip replacement comprise dislocation, infection, peri-prosthetic fracture, limpingwhich are managed accordingly.
References
1. Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med 2004; 351: 1645-1654.
2. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969; 51: 737-55.
3. Marchetti P, Binazzi R, Vaccari V, Girolami M, Morici F, Impallomeni C, et al. Long-term results with cementless Fitek (or Fitmore) cups. J Arthroplasty 2005; 20: 730-7.
4. Hawker GA, Wright JG, Coyte PC, Williams JI, Harvey B, Glazier R, et al. Differences between men and women in the rate of use of hip and knee arthroplasty. N Eng J Med 2000; 342: 1016-1022.
5. Mahomed N, Gandhi R, Daltroy L, Katz JN. The self-administered patient satisfaction scale for primary hip and knee arthroplasty. Arthritis 2011; 2011: 591253. doi: 10.1155/2011/591253.
6. Ranawat CS, Atkinson RE, Salvati EA, Wilson PD Jr. Conventional total hip arthroplasty for degenerative joint disease in patients between the ages of forty and sixty years. J Bone Joint Surg Am 1984; 66: 745-52.
7. Archibeck MJ, Berger RA, Jacobs JJ, Quigley LR, Gitelis S, Rosenberg AG, et al. Second-generation cementless total hip arthroplasty. Eight to eleven-year results. J Bone Joint Surg Am 2001; 83: 1666-1673.
8. Shahab ud Din, Ahmed I, Hayat S. Cemented total hip replacement in patients younger than 50 years of age. J Postgrad Med Inst 2005; 19: 416-9.
9. Berli BJ, Ping G, Dick W, Morscher EW. Nonmodular flexible press-fit cup in primary total hip arthroplasty: 15-year followup. Clin Orthop Relat Res 2007; 461: 114-21.
10. Ragab AA, Kraay MJ, Goldberg VM. Clinical and radiographic outcomes of total hip arthroplasty with insertion of an anatomically designed femoral component without cement for the treatment of primary osteoarthritis. A study with a minimum of six years of follow-up. J Bone Joint Surg Am 1999; 81: 210-8.
11. Todkar M. Obesity does not necessarily affect the accuracy of acetabular cup implantation in total hip replacement. Acta Orthop Belg 2008; 74: 206-9.
12. Nixon M, Taylor G, Sheldon P, Iqbal SJ, Harper W. Does bone quality predict loosening of cemented total hip replacements? J Bone Joint Surg Br 2007; 89: 1303-8.
13. Hailer NP, Lazarinis S, Mäkelä KT, Eskelinen A, Fenstad AM, Hallan G, et al. Hydroxyapatite coating does not improve uncemented stem survival after total hip arthroplasty! Acta Orthop 2015; 86: 18-25.
14. Ng CY, Ballantyne JA, Brenkel IJ. Quality of life and functional outcome after primary total hip replacement: a five-year follow-up. J Bone Joint Surg Br 2007; 89: 868-73.
15. SooHoo NF, Farng E, Zingmond DS. Disparities in the utilization of high-volume hospitals for total hip replacement. J Natl Med Assoc 2011; 103: 31-35.
16. MacDonald SJ, McCalden RW, Chess DG, Bourne RB, Rorabeck CH, Cleland D, et al. Metal-on-metal versus polyethylene in hip arthroplasty: a randomized clinical trial. Clin Orthop Relat Res 2003; 406: 282-96.
17. Trudelle-Jackson E, Emerson R, Smith S. Outcomes of total hip arthroplasty: a study of patients one year postsurgery. J Orthop Sports Phys Ther 2002; 32: 260-267.
18. Bruyère O, Ethgen O, Neuprez A, Zégels B, Gillet P, Huskin JP, et al. Health-related quality of life after total knee or hip replacement for osteoarthritis: a 7-year prospective study. Arch Orthop Trauma Surg 2012; 132: 1583-7.
19. Pierce TP, Jauregui JJ, Cherian JJ, Elmallah RD, Robinson K, Mont MA. Prospective evaluation of short and mid-term outcomes of total hip arthroplasty using the Accolade TM stem. Hip Int 2015:0. doi: 10.5301/hipint.5000238.
20. Kim Y, Tanaka C, Tada H, Kanoe H, Shirai T. Treatment of peri-prosthetic femoral fractures after femoral revision using a long stem. BMC Musculoskelet Disord 2015; 16: 113. doi:10.1186/s12891-015-0565-7
21. Loudon JR, Charnley J. Subsidence of the femoral prosthesis in total hip replacement in relation to the design of the stem. J Bone Joint Surg Br 1980; 62: 450-3.
22. Turpie AG, Gallus AS, Hoek JA; Pentasaccharide Investigators. A synthetic pentasaccharide for the prevention of deep-vein thrombosis after total hip replacement. N Engl J Med 2001; 344: 619-25.
23. Eriksson BI, Dahl OE, Rosencher N, Kurth AA, van Dijk CN, Frostick SP, et al. Dabigatran etexilate versus enoxaparin for prevention of venous thromboembolism after total hip replacement: a randomised, double-blind, non-inferiority trial. Lancet 2007; 370: 949-56.
Journal of the Pakistan Medical Association has agreed to receive and publish manuscripts in accordance with the principles of the following committees:




