Muhammad Jamaluddin ( Surgical Unit-1, Karachi Medical and Dental College and Abbasi Shaheed Hospital, Karachi. )
Syed Mohammad Abbas Hussain ( Surgical Unit-1, Karachi Medical and Dental College and Abbasi Shaheed Hospital, Karachi. )
Humaid Ahmad ( Surgical Unit-1, Karachi Medical and Dental College and Abbasi Shaheed Hospital, Karachi. )
November 2013, Volume 63, Issue 11
Original Article
Abstract
Objective: To study the role of hyperbilirubinaemia as a predictive factor for appendiceal perforation in acute appendicitis.
Methods: The prospective, descriptive study was conducted at the Abbasi Shaheed Hospital and the Karachi Medical and Dental College, Karachi, from January 2010 to June 2012. It comprised all patients coming to the surgical outpatient department and emergency department with pain in the right iliac fossa with duration less than seven days. They were clinically assessed for signs and symptoms of acute appendicitis and relevant tests were conducted. Patients were diagnosed as a case of acute appendicitis on the basis of clinical and ultrasound findings, and were prepared for appendicectomy. Per-operative findings were recorded and specimens were sent for histopathology to confirm the diagnosis. SPSS version 10 was used to analyse the data.
Results: Of the 71 patients, 37 (52.10%) were male and 34 (47.90%) were female. The age range was 3-57 years, and most of the patients (n=33; 46.5%) were between 11 and 20 years. Besides, 63 (89%) patients had pain in the right iliac fossa of less than four-days duration, while 8 (11%) had pain of longer duration. Total leukocyte count was found to be elevated in 33 (46.5%) patients, while total serum bilirubin was elevated in 41 (57.70%). Ultrasound of abdomen showed 9 (12.70%) patients having normal appearance of appendix and 59 (83.30%) had inflamed appendix. Four (5.60%) patients had no signs of inflammation on naked eye appearance per operatively. Histopathology of appendix showed 10 (14.10%) patients had non-inflammatory appendix.
Conclusion: Patients with signs and symptoms of acute appendicitis and a raised total serum bilirubin level indicated a complication of acute appendicitis requiring an early intervention to prevent peritonitis and septicaemia. A raised serum bilirubin level is a good indicator of complicated acute appendicitis, and should be included in the assessment of patients with suspected complicated acute appendicitis.
Keywords: Acute appendicitis, Hyperbilirubinaemia, Gangrene, Appendicectomy. (JPMA 63: 1374; 2013).
Introduction
Acute appendicitis (AA) is one of the most frequent pathologies among surgical illnesses. Diagnosis is easy in typical cases, but difficult in atypical cases.1 Diagnosis of AA remains a surgical dilemma, with negative appendectomy rates of 5% to 40% and perforation suggestive for late operative intervention in 5% to 30%.2 Traditionally, the AA diagnosis has been based mainly on a history compatible with AA and pain at McBurney\\\'s point. Determining the optimum algorithm for diagnostic procedure in suspected AA may not only reduce the number of unnecessary operations, but also the frequency of complications, and may contribute significantly to reducing the cost of treating patients with acute abdominal conditions.3 Therefore, delay in diagnosis or treatment of AA may lead to serious life-threatening conditions like gangrene and perforation of appendix leading to peritonitis. Hyperbilirubinaemia is the result of imbalance between production and excretion of bilirubin by the liver. It may be because of hepatocellular, cholestatic or haemolytic diseases. Portal blood carries nutrients and other substances absorbed from the gut, including bacteria and its product (toxins). In a small percentage, even in normal healthy people, bacteria are found in portal blood. It is commonly cleared by detoxification and immunological action of reticuloendothelial (RES) system of liver that acts as firstline defense in clearing toxic substances, bacteria and its products. But when bacterial load overwhelms the Kupffer cell function, it may cause dysfunction or damage to the hepatocytes (liver parenchyma). It reflects rise in serum bilirubin (SB) alone or in combination with liver enzymes depending upon the type, severity and site of lesion.4 Escherichia coli endotoxin has been shown to impact physiological bile flow in vivo.5 This had led to the theory that hyperbilirubinaemia in patients with appendicitis may have a predictive potential for the pre-operative diagnosis of appendiceal perforation. But no reliably specific marker for AA has been identified. Although recent studies have shown hyperbilirubinaemia to be a useful predictor of appendiceal perforation, but they did not focus on the value of bilirubin as a marker for acute appendicitis.6 Therefore, the aim of this study was to determine the value of hyperbilirubinaemia as a marker for complication of AA like gangrene and perforation of the appendix.
Patients and Methods
The prospective, descriptive study was conducted at Abbasi Shaheed Hospital and Karachi Medical and Dental College, Karachi, from January 2010 to June 2012. All patients presenting to the surgical outpatient department (OPD) and emergency department (ED) during the study period with pain in the right iliac fossa with duration less than seven days were included. They were clinically assessed for signs and symptoms of AA. The diagnosis was made on the basis of history, clinical examination like tenderness and rebound tenderness in the right iliac fossa, and lab reports including haemoglobin (Hb.%), while blood cell (WBC) count, total bilirubin level, blood sugar, Urine detail report and ultrasound of abdomen. Patients having chronic liver disease, those with lump in the right lower quadrant, pregnancy or hepatitis B and C reactive were excluded. All patients diagnosed as a case of AA were prepared for appendicectomy. They were informed about the study and a written consent was obtained. Prophylactic antibiotic, third-generation cephalosporin along with metronidazole were given before the induction of anaesthesia. All patients were operated in the emergency operation theatre and per-operative findings were recorded and specimens were sent for histopathology to confirm the diagnosis. SPSS version 10 was used to analyse the data.
Results
Of the total 71 patients, 37 (52.10%) were male and 34 (47.90%) were female (Table-1). The age range 3-57 years and most of the patients (n=33; 46.5%) were between 11 and 20 years (Figure-1).
The age range 3-57 years and most of the patients (n=33; 46.5%) were between 11 and 20 years (Figure-1).
Besides, 63 (89%) patients had pain in the right iliac fossa of less than four-days duration, while 8 (11.20%) had pain of longer duration (Table-2).
Total leukocyte count was found to be elevated in 33 (46.50%) patients and within normal range in 38 (53.50%). Total SB was found to be elevated in 47 (57.70%) patients and within normal range in 30 (43.30%) (Figure-2).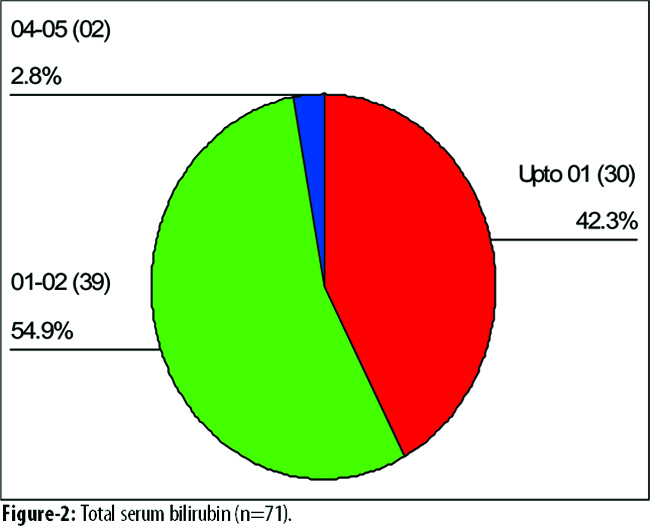
Ultrasound of abdomen showed 9 (12.7%) patients having normal appearance of appendix, and 59 (87.30%) with inflamed appendix with or without any free fluid. Per-operatively, 4 (5.60%) patients had no signs of inflammation on naked eye appearance, while 25 (35.20%) had moderate to severe signs of inflammation without gangrene or perforation, and 42 (59.20%) had severe signs of inflammation with gangrene and perforation of appendix (Figure-3).
Histopathology of appendix showed 10 (14.10%) patients had non-inflammatory appendix, 20 (28.20%) had moderate to severe inflammation without gangrene or perforation, and 41 (57.70%) had severe inflammation with gangrene or perforation of the appendix (Figure-4).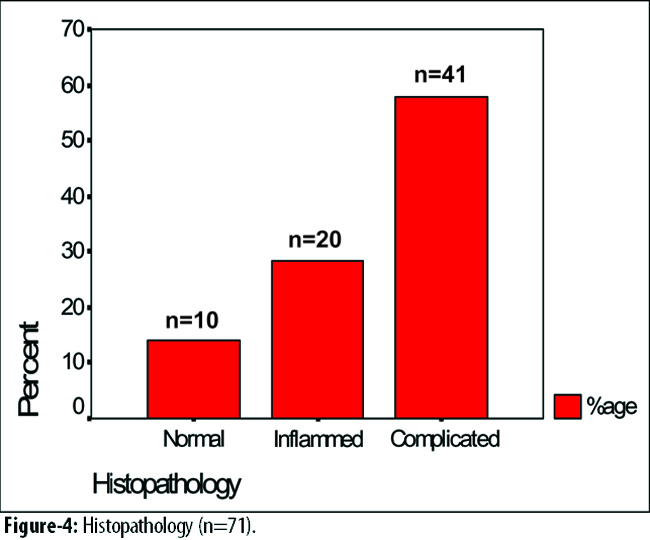
Overall, 41 (57.70%) patients had elevated SB (Figure-5).
Discusions
The main features of AA including pain in the right iliac fossa, duration of pain, tenderness, rebound tenderness, temperature, diagnostic modalities like ultrasound of abdomen, total leukocyte count and SB level, and operative and histopathologic findings of the appendix were studied. It was found that most of the patients were between 11 to 20 years of age, while only a few patients were above 30 years which is similar to earlier studies.3,7 Majority of the patients in this study were male which is similar to a study conducted in Turkey.8 The main presenting feature was pain in the right iliac fossa in this study, while the classical pain in AA is felt in periumbilical or epigastric region which shifts to the right iliac fossa.9 The majority of the patients in our study presented with pain mainly for four days and only 11.20% of patients presented with pain between five and seven days. Some studies showed the time of presentation to be 24 to 48 hours10 while others showed less than four days.11 Total leukocyte count was within normal range in 53.50% of patients, which is similar to a study conducted in Nepal,12 while 46.50% of the patients in this study showed a raised total leukocyte count which is similar to most other studies.13 Some researchers also showed that total leukocyte count is not reliable and may be normal in AA.2,14,15 The diagnosis of AA was made mainly on the basis of history and clinical examinations and supported by ultrasound of abdomen, total leukocyte count, while in other studies computed tomography and magnetic resonance imaging (CT/MRI) scans were required to diagnose the case.16 Total SB level was found to be elevated in 57.70% patients which is similar to most studies.8,17 In the current study, 57.7% patients with hyperbilirubinaemia had gangrenous or perforated appendix, which is similar to earlier studies.6,18 Per-operative findings in this study showed that only 5.6% patients had normal-looking appendix, while most of the patients had moderate to severe inflammation of the appendix. Other studies showed that normal-looking appendicectomy rate is 8.2%,3 while in some centres it was 15 to 20%19 which is quite high compared to our study. The histopathology confirmed that 85.9% patients had inflamed appendix in this study, while most other studies showed fewer than this result7,20 and a study in the United Kingdom showed only 75.4% positive histopathology result.21 In our study only 14.1% patients had non-inflamed appendix, while majority of the studies showed quite different results from 5% to 25%22,23 which indicates that the clinical experience is more important than the costly investigations. Different studies tried different investigations to diagnose AA3,24 and to minimise the chances to operate on a normal appendix,25 but it is clear from this study that history and clinical examination are the main diagnostic tools for simple AA which may be supported by an ultrasound of the abdomen,26 but some studies showed that the sensitivity of leukocyte count was significantly higher than that of ultrasound in the diagnosis of AA.1,27 Other studies also indicated that CT is superior in the diagnosis of AA.25 It is also evident from our study that AA with complications like gangrene or perforation of the appendix may be suspected if patients has a raised SB level along with a raised total leukocyte count,8,28 but some studies also showed that AA may be diagnosed with a normal leukocyte count.2,29 From this study, it is also evident that almost all AA patients having complications like gangrene and perforation have raised SB. The success rate in diagnosing complicated AA by history, clinical examination and using diagnostic modality like SB level was more than 90% in this study which is quite high compared to other studies.3
Conclusion
A raised SB level is a good indicator of complicated AA and patients with hyperbilirubinaemia are more likely to have appendiceal perforation or gangrene. A total SB level investigation should be included in the assessment of patients with suspected complicated AA.
References
1. Demircan A, Aygencel G, Karamercan M, Ergin M, Yilmaz TU, Karamercan A. Ultrasonographic findings and evaluation of white blood cell counts in patients undergoing laparotomy with the diagnosis of acute appendicitis. Ulus Travma Acil Cerrahi Derg 2010; 16: 248-52.
2. Thuijls G, Derikx JP, Prakken FJ, Huisman B, van Bijnen Ing AA, van Heurn EL, et al. A pilot study on potential new plasma markers for diagnosis of acute appendicitis. Am J Emerg Med 2011; 29: 256-60.
3. Anielski R, Kusnierz-Cabala B, Szafraniec K. An evaluation of the utility of additional tests in the preoperative diagnostics of acute appendicitis. Langenbecks Arch Surg 2010; 395: 1061-8.
4. Khan S. Evaluation of hyperbilirubinemia in acute inflammation of appendix: a prospective study of 45 cases. Kathmandu Univ Med J 2006; 4: 281-9.
5. Sand M, Bechara FG, Holland-Letz T, Sand D, Mehnert G, Mann B. Diagnostic value of hyperbilirubinemia as a predictive factor for appendiceal perforation in acute appendicitis. Am J Surg 2009; 198: 193-8.
6. Emmanuel A, Murchan P, Wilson I, Balfe P. The value of hyperbilirubinaemia in the diagnosis of acute appendicitis. Ann R Coll Surg Engl 2011; 93: 213-7.
7. Xharra S, Gashi-Luci L, Xharra K, Veselaj F, Bicaj B, Sada F, et al. Correlation of serum C-reactive protein, white blood count and neutrophil percentage with histopathology findings inacute appendicitis. World J Emerg Surg 2012;7:27. doi: 10.1186/1749-7922-7-27.
8. Atahan K, Üreyen O, Aslan E, Deniz M, Çökmez A, Gür S, et al. Preoperative diagnostic role of hyperbilirubinaemia as a marker of appendix perforation. J Int Med Res 2011; 39: 609-18.
9. Lee SI, Ho HS. Acute appendicitis: is there any difference between children and adult? Am Surg 2006; 72: 409-13.
10. Guraya SY, Al-Tuwaijri TA, Khairy GA, Murshid KR. Validity of leukocyte count to predict the severity of acute appendicitis. Saudi Med J 2005; 26: 1945-7.
11. Kharbanda AB, Rai AJ, Cosme Y, Liu K, Dayan PS. Novel serum and urine markers for pediatric appendicitis. Acad Emerg Med 2012; 19: 56-62.
12. Agrawal CS, Adhikari S, Kumar M. Role of serum C-reactive protein and leukocyte count in the diagnosis of acute appendicitis in Nepalese population. Nepal Med Coll J 2008; 10: 11-5.
13. Bilici S, Sekmenli T, Göksu M, Melek M, Avci V. Mean platelet volume in diagnosis of acute appendicitis in children. Afr Health Sci 2011; 11: 427-32.
14. Yazici M, Ozkisacik S, Oztan MO, Gürsoy H. Neutrophil/lymphocyte ratio in the diagnosis of childhood appendicitis. Turk J Pediatr 2010; 52: 400-3.
15. Kamran H, Naveed D, Nazir A, Hameed M, Ahmed M, Khan U. Role of total leukocyte count in diagnosis of acute appendicitis. J Ayub Med Coll Abbottabad 2008; 20: 70-1.
16. Kim HC, Yang DM, Lee CM, Jin W, Nam DH, Song JY, et al. Acute appendicitis: relationships between CT-determined severities and serum white blood cell counts and C-reactive protein levels. Br J Radiol 2011; 84: 1115-20.
17. Sand M, Bechara FG, Holland-Letz T, Sand D, Mehnert G, Mann B. Diagnostic value of hyperbilirubinemia as a predictive factor for appendiceal perforation in acute appendicitis. Am J Surg 2009; 198: 193-8.
18. Käser SA, Fankhauser G, Willi N, Maurer CA. C-reactive protein is superior to bilirubin for anticipation of perforation in acute appendicitis. Scand J Gastroenterol 2010; 45: 885-92.
19. Grönroos JM. Clinical suspicion of acute appendicitis - is the time ripe for more conservative treatment? Minim Invasive Ther Allied Technol 2011; 20: 42-5.
20. Johansson EP, Rydh A, Riklund KA. Ultrasound, computed tomography, and laboratory findings in the diagnosis of appendicitis. Acta Radiol 2007; 48: 267-73.
21. Mekhail P, Naguib N, Yanni F, Izzidien A. Appendicitis in paediatric age group: correlation between preoperative inflammatory markers and postoperative histological diagnosis. Afr J Paediatr Surg 2011; 8: 309-12.
22. Gendel I, Gutermacher M, Buklan G, Lazar L, Kidron D, Paran H, et al. Relative value of clinical, laboratory and imaging tools in diagnosing pediatric acute appendicitis. Eur J Pediatr Surg 2011; 21: 229-33.
23. Müller AM, Kaucevic M, Coerdt W, Turial S. Appendicitis in childhood: correlation of clinical data with histopathological findings. Klin Padiatr 2010; 222: 449-54.
24. Singh-Ranger D, Ogadegbe A. Leucocyte count and oral temperature are a useful guide to selecting women with right iliac fossa pain for diagnostic laparoscopy. Ann R Coll Surg Engl 2010; 92: 425-8.
25. Merlin MA, Shah CN, Shiroff AM. Evidence-based appendicitis: the initial work-up. Postgrad Med 2010; 122: 189-95.
26. Butala P, Greenstein AJ, Sur MD, Mehta N, Sadot E, Divino CM. Surgical management of acute right lower-quadrant pain in pregnancy: a prospective cohort study. J Am Coll Surg 2010; 211: 490-4.
27. Kiyak G, Korukluoglu B, Ozgün Y, Devay AO, Kusdemir A. Evaluation of Ohmann and Eskelinen scores, leukocyte count and ultrasonography findings for diagnosis of appendicitis. Ulus Travma Acil Cerrahi Derg 2009; 15: 77-81.
28. Estrada JJ, Petrosyan M, Barnhart J, Tao M, Sohn H, Towfigh S, et al. Hyperbilirubinemia in appendicitis: a new predictor of perforation. J Gastrointest Surg 2007; 11: 714-8.
29. Grönroos P, Huhtinen H, Grönroos JM. Normal leukocyte count and C-reactive protein value do not effectively exclude acute appendicitis in children. Dis Colon Rectum 2009; 52: 1028-9.
Related Articles
Journal of the Pakistan Medical Association has agreed to receive and publish manuscripts in accordance with the principles of the following committees:




